
Accounting for approx. 24 %, SSIs are the most frequent nosocomial infections in German acute-care hospitals, while the risk of infection depends on the type of operation. Bacteria, rarely in combination with fungi, are the most common pathogens of an SSI, and the spectrum of pathogens varies depending on the surgical site and type of operation, respectively. Based on the OP-KISS (German surgical site infection surveillance) data from 2010 to 2014, the Robert Koch-Institute reports the following bacteria shares for selected surgical procedures1:
Most frequent pathogens of surgical site infections (SSI) for selected types of surgery
| Pathogen | Abdominal surgery |
Heart surgery | Traumatology/orthopaedics |
All surgeries |
|---|---|---|---|---|
| Staphylococcus aureus | 4% | 25% | 32% | 20% |
| Enterococcus spp. | 29% | 10% | 11% | 18% |
| Escherichia coli | 30% | 5% | 5% | 15% |
| Coagulase-negative staphylococci (CoNS) as the sole pathogen |
1% | 21% | 17% | 10% |
| Pseudomonas aeruginosa | 6% | 3% | 3% | 4% |
Effective prevention of SSIs depends on a coordinated mix of appropriate hygienic behaviour, accompanying perioperative measures (before, during and after surgery) and spatial/structural conditions — defined based on the respective SSI risk.
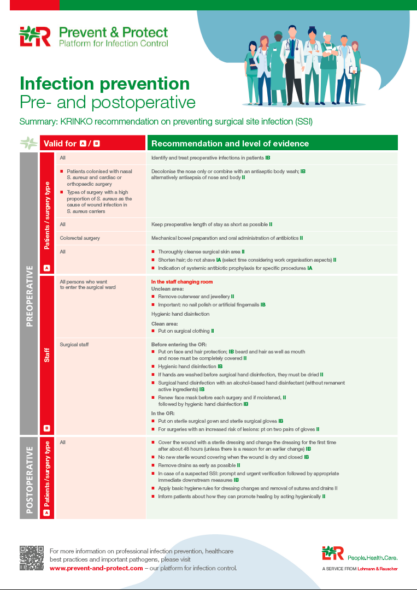
| Infection prevention Pre- and postoperative |
Infection prevention – Intraoperative, between surgeries and at the end of the day |
 |
 |
| Poster download – (2 MB) | Poster download – (2 MB) |

Although surgical techniques have advanced remarkably, operating theatres have become more ergonomic and bundled measures have been implemented, surgical site infection is still a significant burden on the healthcare system. Consequently, an empowered and active role of patients can be an additional and helpful element in preventing surgical site infection. With this in mind, a renowned panel of experts has compiled pragmatic recommendations for patients that cover pre-, intra- and post-operative activities. The result is a patient information leaflet with evidence-based recommendations for practice.
In compiling the information leaflet, the experts focused on providing patients as early as possible in their journey from preparation for surgery to post-operative care with basic and easy-to-implement recommendations that enable them to actively participate in their “patient journey”. The sheet can be both translated into other languages and adapted to local conditions, making it a versatile tool for communication and education.
Healthcare workers can use the patient information leaflet to educate patients and support patient engagement. And for hospitals, it offers an opportunity to complement multidisciplinary prevention strategies by involving patients in preventing infections.
Click here for the expert panel’s “Patient Information Leaflet”.
[1] Prävention postoperativer Wundinfektionen: Empfehlung der Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) beim Robert Koch-Institut. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018 Apr;61(4):448-473