Joint replacement surgeries are of significant therapeutic benefit for many patients, relieving pain and improving mobility. However, the advantages of such surgeries can be greatly hampered by orthopaedic surgical site infections (SSIs), which are associated with high patient morbidity. Reduction of the SSI-associated risk factors and strict adherence to infection control protocols before, during and after surgery are crucial to minimise infections and ensure a positive outcome.
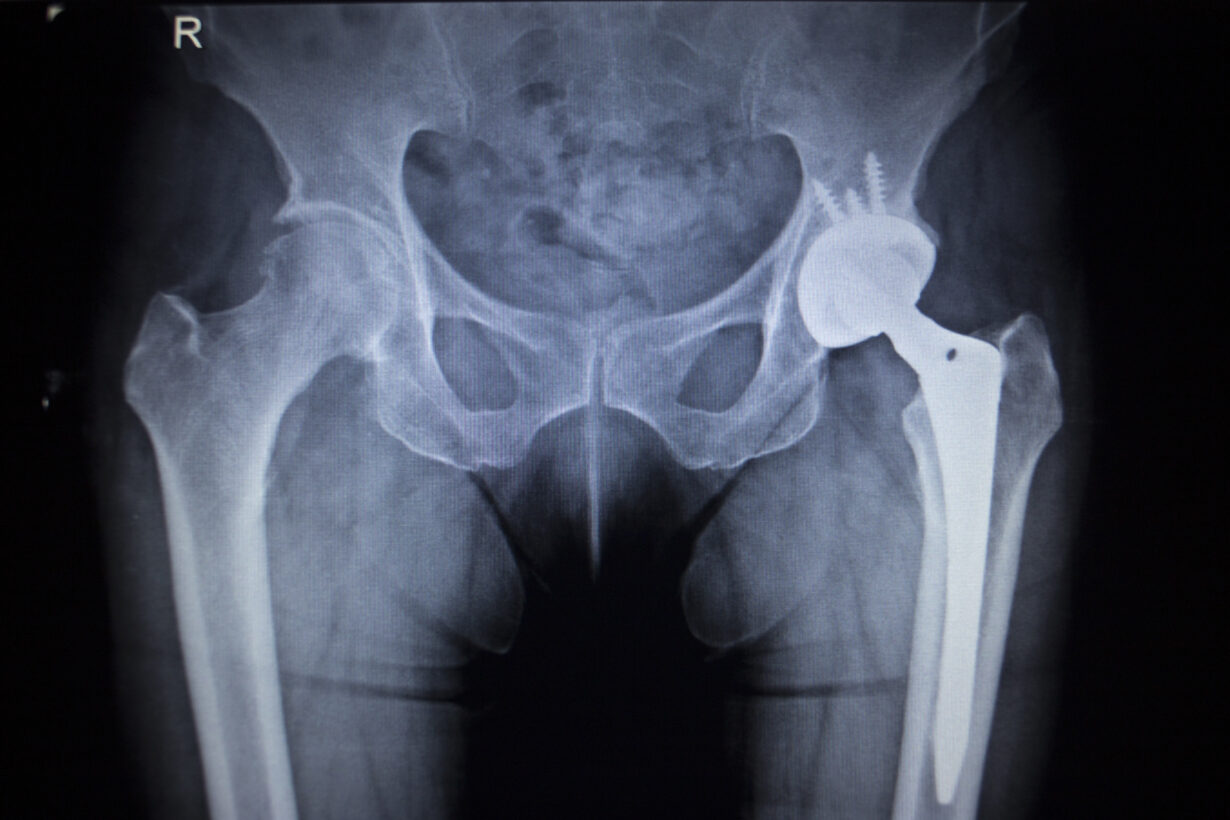
Named "the operation of the century", total hip replacement surgery has revolutionised the lives of millions of patients since its introduction in the 1960s1. With this implant, patients who could barely walk regain a full range of motion and feel “normal” again. Today, joint replacement surgery, such as hip and knee replacement, is one of the most effective interventions for some musculoskeletal conditions. Such surgeries allow both young and elderly patients to reduce pain, restore quality of life and return to physically demanding activities.
For these reasons, the incidence of total joint replacements is high, with over 1 million procedures in the United States, for example, and almost 430,000 procedures in Germany each year2 3. These figures are expected to rise in the near future due to the growing patient demand for improved mobility. Future projections predict an increase of the number of procedures to over 4 million by the year 2040, making joint replacement the most common elective surgical procedure in the near future4.
However, this rapid increase in patients alongside the concomitant aging population, the growing prevalence of obesity and other metabolic disorders could lead to a higher incidence of post-surgical complications, and primarily surgical site infections (SSIs)5. Surgical site infections are, in fact, one of the most frequent and threatening complications following insertion of hip or knee prostheses, creating considerable challenges for patients and healthcare personnel6. As only one example, orthopaedic SSIs are a major cause of morbidity and mortality. They also increase the length of hospital stays; the financial burden of such extended stays also cause physical and psychological suffering for patients. Finally, orthopaedic SSIs have long-term effects on patients’ mobility7. More than 25 percent of revision surgeries after arthroplasty are attributed to SSIs, and those also bear further risks of infection8.
Make sure you receive:
When looking at the epidemiological data on microorganisms identified in SSI, it becomes clear that gram-positive cocci such as coagulase-negative staphylococci and (Enterococcus ssp.) are responsible for more than two-thirds of these infections. Gram-negative bacteria are found in 15-19 percent of the SSIs9. Methicillin-resistant Staphylococcus aureus (MRSA) account for 10 to 25 percent of SSIs after arthroplasty, and nasal colonisation by this pathogen increases the risk for SSIs10. In fact, the growing incidence of antimicrobial resistance represents such a significant issue that it threatens to undermine the advantages of the surgery.
Data from the 2017 Annual Epidemiological Report of the European Centre for Disease Prevention and Control (ECDC) report a mean orthopaedic SSI incidence of 1 percent in hip prosthesis surgeries and 0.5 percent in knee prosthesis surgeries11. After revision, the incidence can rise up to 5 percent due to the more extensive surgical approach5. Even if these figures suggest a low risk of infection, they become significant when looking at the increasing number of surgeries and the devastating consequences. Therefore, it is crucial to identify and reduce the risk factors for orthopaedic SSIs and improve infection prevention and control measures.
The risk of developing an infection after arthroplasty depends on a variety of factors; these can be related to the patient, the surgical procedure or to the implant itself. Some of these factors can be modified, while others cannot be influenced. A meta-analysis of 2017 found that the main patient-related factors associated with orthopaedic SSIs were male gender, age, obesity, uncontrolled diabetes mellitus, urinary tract infections, alcohol abuse and rheumatoid arthritis. Poor nutritional status resulted in adverse outcomes after arthroplasties, mainly due to poor wound healing and increased infection rates.
As well, an American Society of Anesthesiologists (ASA) scale?greater than 2 is considered a high-risk factor. This score is used to assess the general health of patients before surgery, and a score higher than 2 indicates severe systemic diseases. Drain usage, on the other hand, had a protective effect for the patients12. Moreover, the length of surgery also negatively influenced the incidence of SSIs after joint replacement13. Considering some of these risk factors, it becomes clear that the worldwide increasing prevalence of diseases such as adiposities and diabetes, as well as an ageing population, negatively contribute to the incidence of periprosthetic joint infections14.
In order to avoid the sometimes devastating complications of SSIs after joint replacements, enhanced prevention measures before, during and after surgery need to be implemented, especially considering that eradication of infection can be very difficult15. Pre-operative methods include a strict management of the patient-specific risk factors and hygienic measures such as showering and therapy for existing infections. Potential infectious foci on the skin and in the mouth should also be treated. As patients testing positive for nasal Staphylococcus aureus colonisation have a three to six times higher infection risk than non-carriers, screening and decolonisation are also indicated. Finally, the advantages of prophylactic antibiotic therapy short before joint replacement surgery are also recognised.
During surgery strict adherence to hygienic protocols, which regulate surgical hand preparation16, wearing surgical scrubs°, masks°, gowns° and gloves°, and disinfection of surfaces°, is mandatory. In order to further decrease the risk of contamination due to glove perforation, many surgeons use a double glove in the operative environment, appropriate ventilation systems and reduction of traffic in the operating room; correct surgical techniques are also required to avoid microbial contamination. There are also several reports stating that adding antibiotics to cement can decrease the risk of prosthetic joint infections17.
After surgery, careful assessment and follow-up of the operative wound are important for an early detection of eventual infection signs. The use of anticoagulants and the choice of wound dressing° depend on the local protocols and differ among the different surgical departments. At the moment there is no clear evidence for the superiority of one dressing over others18.

Since infections often have multiple causes, individual measures are often not sufficient to prevent them. This is the reason why combining several individual measures might prove more effective for preventing SSIs after joint replacement. These bundles could include procedures to be followed by the surgical team and/or the patient before, during and after the operation. In this context, educating the patients before a planned operation is key for increasing their safety19.
In 2018 Germany’s Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) released recommendations for the prevention of SSIs which aim at ensuring standardisation of the infection control procedures. In these guidelines the commission makes SSI surveillance measures mandatory as they are a key component for the prevention of healthcare-associated infections and an important tool for monitoring the effectiveness of prevention and control measures. These guidelines also provide updated evidence-based recommendations to prevent SSIs and give surgeons guidance about useful surveillance practices20. These measures reflect that regular surveillance of SSIs can significantly contribute to a decreasing risk of infections after surgical procedures21.
Given the traumatising consequences of orthopaedic SSIs after joint replacement surgeries, minimisation of risks, correct surgical techniques, minimisation of surgical duration procedures, usage of implants with low bacterial adhesion22 and bundling several infection prevention interventions are all crucial to reduce the incidence of infections. To ensure the intended result for a growing number of patients, procedures should therefore be carried out using standardised protocols and following guidelines.
Further information
°Commercial communication