“Thanks for reminding me”- The cultural change in hand hygiene
In a stressful working day, healthcare professionals might forget to clean their hands every time it is necessary.... read more

Hand hygiene is still not sufficiently and consistently implemented. According to a recent study, one possible reason is that medical personnel do not seem to be aware of how often they touch patients, and the surfaces inside and outside of the patient’s environment. Such contacts can transmit microorganisms and create potential risks of infection. The study found that on average, contact takes place every 4.2 seconds during patient care and treatment – and every two minutes, even contact that carries the risk of infection.
First greet the patient. Then place medical equipment you’ve brought with you onto the patient’s bedside table. Check the vein access site in the patient’s arm. Then check the infusion bag. Make a note of the medication in the patient’s file. Touch the pocket of your coat because your station pager beeps. Feel the patient’s pulse. Change the wound dressing*, brushing back a strand of hair that has slipped into your face.
Many such contacts take place between nurses or doctors and their patients or their environments. All carry a potential risk of infection if your hands are not disinfected before any contact with so-called critical areas (e.g. wounds, mucous membranes, infusion accesses).
Nevertheless, hand hygiene is not sufficiently and consistently implemented at such moments. To clarify and quantify the topic, a team led by Lauren Clack and Hugo Sax from the Division of Infectious Diseases and Hospital Epidemiology at Zurich University Hospital investigated how many such contacts occur between the hands of staff, patients, and various surfaces in everyday intensive care.
The researchers discovered that on average, a transmission of potentially harmful microorganisms to the patient and his environment occurs every four seconds, and a potentially infectious contact approximately every two minutes.
The authors published their results in the journal “Antimicrobial Resistance & Infection Control“ in 2017.1 The team observed patient-surface contacts in three intensive care units for trauma, cardiac and visceral surgery using head-mounted cameras. The camera angle was adjusted to keep the hands of the participants – eight nurses and two doctors – permanently in the field of view. Each of the ten subjects wore the camera system for 70 minutes during their morning shift.
Following the videotaping, the researchers selected approximately 30 minutes of each video sequence involving direct patient care, and evaluated the data for contamination and infection risks. The scientists evaluated all hand-to-surface contacts in the respective video sequences and coded them with regard to their number, duration and type. In addition, the researchers recorded which hand the staff member used, which surfaces they touched and whether their hands were gloved*.
The analysis of the research team reveals a problem that is surprising in its scope: When medical staff members are concentrating primarily on care or treatment activities, they do not seem to notice how often they touch surfaces inside and outside the patient’s environment, and with critical areas of the patients.
Perhaps this low awareness is one of the reasons for the poor implementation of hand hygiene, the researchers suspect. In particular, the frequent and mostly unconscious contact of hospital staff with their own bodies and clothing is an unexpected result of the study.
Until now, experts had assumed that the direct patient environment was mainly populated with the patient’s own flora. However, the results of the Swiss study suggest that the patient’s environment is also populated with foreign microorganisms. One reason is the frequent change of nurses’ and doctors’ hands between “inside” and “outside” the patient zone, according to the Swiss researchers.
In detail, the authors of the study sorted the events as follows: Touches “outside the patient’s zone” included, for example, the carer’s body, clothing and equipment, other patients and all other surfaces outside the direct patient environment. “Inside the patient’s zone” included the patient himself and all objects in his immediate vicinity.
“Critical points” included sterile medical devices (such as a catheters or other sterile equipment) that have been brought into the room, and critical parts of the patient’s body that must be rigorously protected against microbial contamination to prevent infection.
The researchers defined touching a surface “outside the patient zone” followed by contact with a surface “inside the patient zone” as a “colonisation event” – i.e. an event in which microorganisms were transferred from outside to inside the patient environment.
Sequences in which any surface was initially touched followed by contact with a “critical” site were defined as an “infection event” – i.e. an event in which microorganisms were transferred from a surface to a part of the patient’s body that required rigorous protection against infection. (See figure below)

During the observation, the researchers counted a total of 4,222 hand-to-surface contacts, including 291 colonization events (6.9 per cent) and 217 infection events (5.1 per cent). Interestingly, 61 per cent of colonization events and 2.3 per cent of infection events occurred following contact with the hospital staff member’s own body (clothing, hair, skin).
This correlation was put into relation to the actual hand disinfection activities: hand hygiene was carried out before only 14 of the 291 colonisation events, and only three of the 217 infection events. This corresponds to a rate of only five per cent and one per cent, respectively.
In addition, the study showed that although hand disinfection was performed every three minutes, it was rarely following colonization or before infection events. In addition, the average actual application time for hand disinfection was only 11 seconds. To ensure sufficient wetting of the hands with disinfectant, however, it takes about 30 seconds.
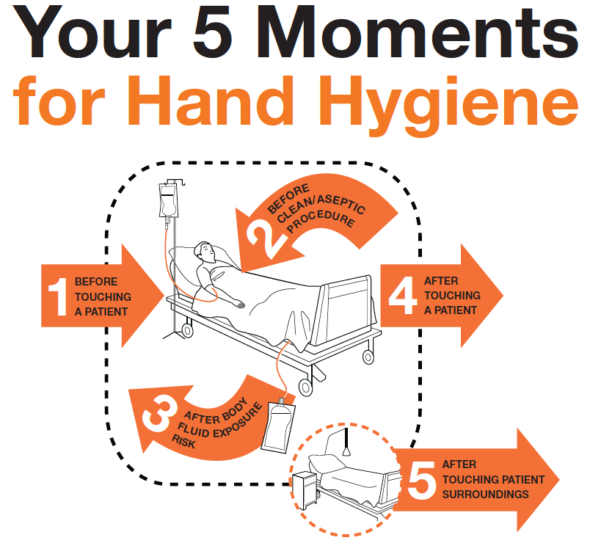
The results of the study show that the previous interpretation of “moments for hand hygiene” as recommended by the WHO 5-moment-model (see figure 2 below2) may have to be extended – also because touching oneself is not yet regarded as a moment of hand hygiene.
The Swiss authors Clack and Sax hope that their study will encourage further improvements in strategies to prevent infections. According to the Commission for Hospital Hygiene and Infection Prevention (KRINKO) of the Robert Koch Institute (RKI)3, an important step in this direction is that disinfectants should be conveniently available wherever they are needed.
At least then there will be no additional time pressure for staff through unnecessarily long distances to the dispensers to carry out the required disinfection , making it easier for them to follow the recommendations and to protect patients as well as themselves.
Further information
“First-person view” of pathogen transmission and hand hygiene – use of a new head-mounted video capture and coding tool, Clack L et al., Antimicrobial Resistance & Infection Control
Five moments for hand hygiene, World Health Organization