Surgical scrubs: Choosing the right clothing improves patients’ safety
Surgical scrubs can aid in containing the spread of microorganisms found on the skin and on clothing worn... read more

Surgical drapes isolate the surgical site from non-sterile areas of the patient’s body and the operating table. They reduce the risk of surgical site infections (SSI). Optimising their barrier function can help to prevent microbial contamination and to improve patients’ safety.
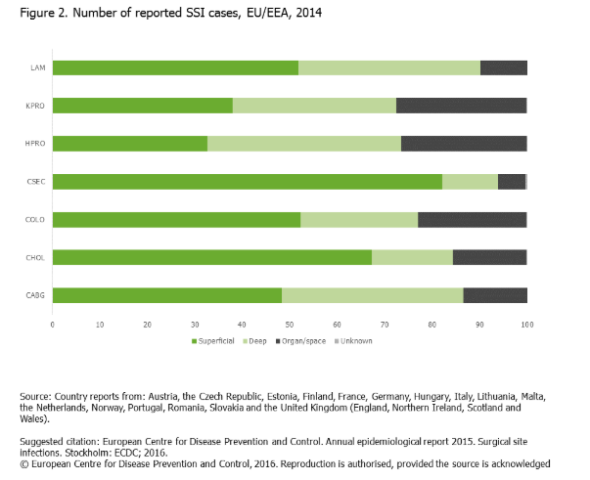
Surgeries are life-saving interventions that are successfully used to treat many conditions such as injuries, cancer, heart diseases and mobility restrictions. Their number rises worldwide every year. According to the German Federal Statistical Office (Statistisches Bundesamt) more than 16.8 million surgeries were performed in Germany in 2017 compared to 13 million a decade earlier. However, along with the increasing number of surgeries, the need for better infection control also rises. Patients need to be protected from surgical site infections (SSI), which account for 22% of healthcare-associated infections (HAI) 1 and are the most frequent type of HAIs in German acute-care hospitals.2 The European Centre for Disease Prevention and Control (ECDC) defines SSI as “postoperative infections occurring within 30 days of a surgical procedure (or within a year for permanent implants)” 3. Minimising the risk of contamination for patients is imperative, as SSI can have severe consequences. Pain, re-admission to the hospital, loss of income, reduced quality of life, and in some cases, death are the human costs suffered by the affected patients. In addition, longer hospitalisation, additional diagnostics measures and treatments substantially increase the financial burden of surgery.4 The treatment of SSIs can also contribute to the spread of antibiotic resistance, one of the biggest threats for healthcare today.
Bacteria such as Staphylococcus aureus, Escherichia coli, coagulase-negative staphylococci, and the Enterococcus species are the most commonly isolated organisms related to SSI5. Methicillin-resistant S. aureus is a relevant source of infection and presents a growing number of challenges for SSI therapy due to multiple antibiotic resistances.
As microorganisms on the patients’ skin are a major source of contamination, using draping materials plays a pivotal role in reducing infections and improving patient outcomes6. Surgical drapes create an effective physical barrier for preventing microbial transfer from both the patient and the environment to the wound.

After antiseptic skin preparation, surgical drapes* are placed over the surgical site to maintain a sterile field and to prevent contact with untreated surfaces. One of their most important features is fluid containment. This is because during surgery, body fluids and irrigating solutions come into contact with the drapes, and the risk for pathogen transmission increases when the materials become moist or wet. Draping material must also be low-lint, as lint can transport microbes and introduce them into the surgical wounds, increasing the risk of infection. Other requirements for sterile surgical drapes include resistance to microbial penetration (dry, wet), the absorption capacity, the resistance to liquid penetration and the tensile strength (according to EN 13795).
Surgical drapes are made of either multiple- or single-use materials, with a wide range of designs and performance characteristics. Reusable materials are composed of tightly woven textiles and/or knitted cotton and can be pre-treated with antimicrobial chemicals. Thread density and chemical treatment are crucial for the barrier properties, which should remain the same after many use-and-cleaning cycles. Disposable materials are composed of non-woven materials of synthetic or natural origins and can also be chemically treated. The potential benefits of reusable drapes include cost and waste reduction, yet these advantages should be compared with the decrease in efficacy at preventing bacterial strikethrough after repeated laundering. Some studies have shown that disposable materials provide superior protection from bacterial strikethrough7.
Still, no national official recommendations exist that suggest the use of either disposable or reusable draping materials, as only limited studies on this topic are available. The 2016 WHO global guidelines on the prevention of SSIs suggest that either disposable non-woven or reusable woven drapes can be used during surgical operations8. However, a prospective randomised study (Showalter BM et al., 20149) analysed the incidence of SSIs in 107 women after implant-based breast reconstruction, which is the most common form of breast reconstruction after a mastectomy. Infections of the implant are here a dreaded complication as they can affect up to 28% of the patients, prolonging treatment and hospitalisation, as well as raising the psychological stress for them. During the study, patients were randomised and allocated either to a group for which reusable drapes were used, or to a group that had disposable drapes during surgery. This was the first study that found a significant benefit in using disposable drapes compared to reusable ones. In the group with reusable drapes, there were five infections in the 30 days following surgery compared to zero in the group with disposable drapes. These findings support the hypothesis that bacterial strikethrough during surgery is more likely with reusable materials.
To find further evidence for clear benefits of disposable versus reusable drapes, more prospective large-scale studies with higher number of patients are needed. In addition, functional requirements, economic aspects and environmental impact need to be taken into account when selecting appropriate drapes for surgery.
FURTHER INFORMATION
*commercial communication